Appointments with your OB-GYN can feel rushed. You’re asked to undress, answer questions, and make big decisions—all in under 20 minutes. But these visits can also be powerful check-ins: a moment to pause, gather insight, and advocate for your body. Whether you’re preparing for pregnancy, navigating new symptoms, or adjusting to postpartum changes, what you ask during your visit can shape the care you receive. At Acumamas, we often encourage our clients to approach these visits not as passive checkups, but as collaborative conversations.
Here are ten thoughtful, grounding questions to consider at your next OB-GYN appointment—so you can leave feeling more informed, more empowered, and more supported in your care.
1. How is my cycle supporting (or hindering) my fertility?
For those thinking about pregnancy—now or in the future—your menstrual cycle offers valuable clues. Irregular periods, heavy bleeding, spotting between cycles, or significant cramping might signal hormonal imbalances or structural issues that impact conception. Ask your OB-GYN to walk you through how your current cycle reflects your reproductive health, and whether further investigation is warranted.
2. What’s the best way to prepare my body for pregnancy?
This question opens the door to personalized preconception care. It might include checking your iron, folate, thyroid function, or vitamin D levels; reviewing your medications; or discussing lifestyle changes that could optimize egg quality or hormone health. At Acumamas, we also collaborate with OB-GYNs to layer in holistic support like acupuncture, nutrition, or gentle detoxification plans.
3. Can we discuss my birth control options in the context of my overall health?
The right birth control should support—not disrupt—your wellbeing. Some options can impact mood, libido, or bleeding patterns. Others might not align with your values or fertility timeline. A thoughtful conversation with your OB-GYN can help you understand how each method interacts with your hormonal rhythm and long-term reproductive goals.
4. Is this pain normal?
Pelvic pain, pain with sex, back pain during periods, or cramping that interferes with daily life are not “just part of being a woman.” They may be signs of conditions like endometriosis, fibroids, or pelvic floor dysfunction. Too often, people are told to tolerate pain that deserves to be explored. Ask directly, and trust your instincts if something doesn’t feel right.
5. What screenings or tests are recommended for someone my age and health history?
From Pap tests to STI screenings to mammograms or hormone panels, the right tests vary by age and medical background. Your OB-GYN can help identify what’s appropriate now and what’s worth monitoring over time. Preventative care isn’t one-size-fits-all—it’s most effective when it’s tailored to you.
6. What support is available if I’m experiencing changes in mood, libido, or energy?
Whether you’re postpartum, perimenopausal, or simply navigating stress, emotional shifts and body changes deserve attention. Mood changes, vaginal dryness, sleep disturbances, or a lack of libido are valid topics to bring up. Your OB-GYN can assess for postpartum depression, hormonal shifts, or other conditions—and can refer you to counseling, physiotherapy, or integrative care, depending on what you need.
7. Can we talk about my pelvic floor?
Most OB-GYN visits don’t include pelvic floor assessment, but they should include pelvic floor awareness. If you’re experiencing leaking, heaviness, pain, or feel disconnected from your core, mention it. While OB-GYNs don’t treat pelvic floor dysfunction directly, they can help rule out other concerns and refer you to a qualified physiotherapist.
8. How does my medical condition or medication affect pregnancy or fertility?
Whether you’re managing PCOS, thyroid disease, diabetes, or autoimmune conditions, it’s important to understand how your health status intersects with reproductive goals. Some medications may require adjustments before trying to conceive. Your OB-GYN can help outline a safe, supportive timeline.
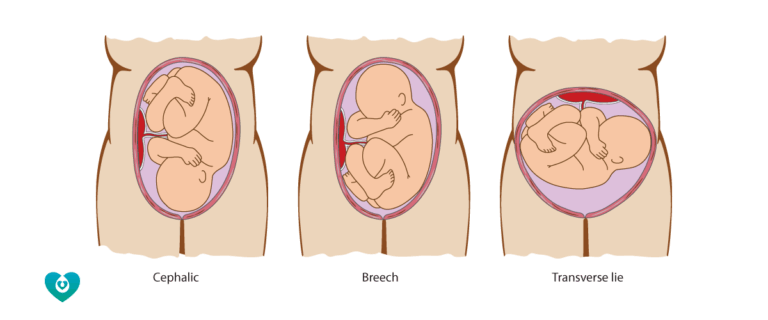
9. What should I expect from labor and birth in the medical system?
Even if you’re early in pregnancy, this is a helpful question. Understanding your OB-GYN’s philosophy around birth, induction, cesarean delivery, and interventions can shape how you build your care team. It also opens the conversation for integrating midwifery care or complementary practices like acupuncture for cervical ripening or labour prep.
10. What can I do to support healing after birth?
Postpartum care is often overlooked, yet it’s one of the most critical windows for long-term health. Ask your OB-GYN about what symptoms are expected, what’s not, and when to seek support. Bring up scar healing, bleeding, bowel function, and mood. You deserve more than a 6-week check—you deserve care that follows through.
Final words
Your OB-GYN visit is more than a checklist—it’s a moment to speak up for what matters most in your care. The right questions can turn a routine appointment into a meaningful exchange. At Acumamas, we believe knowledge is a form of self-care, and we’re here to support you in building a team of care that sees, hears, and honours your whole story.